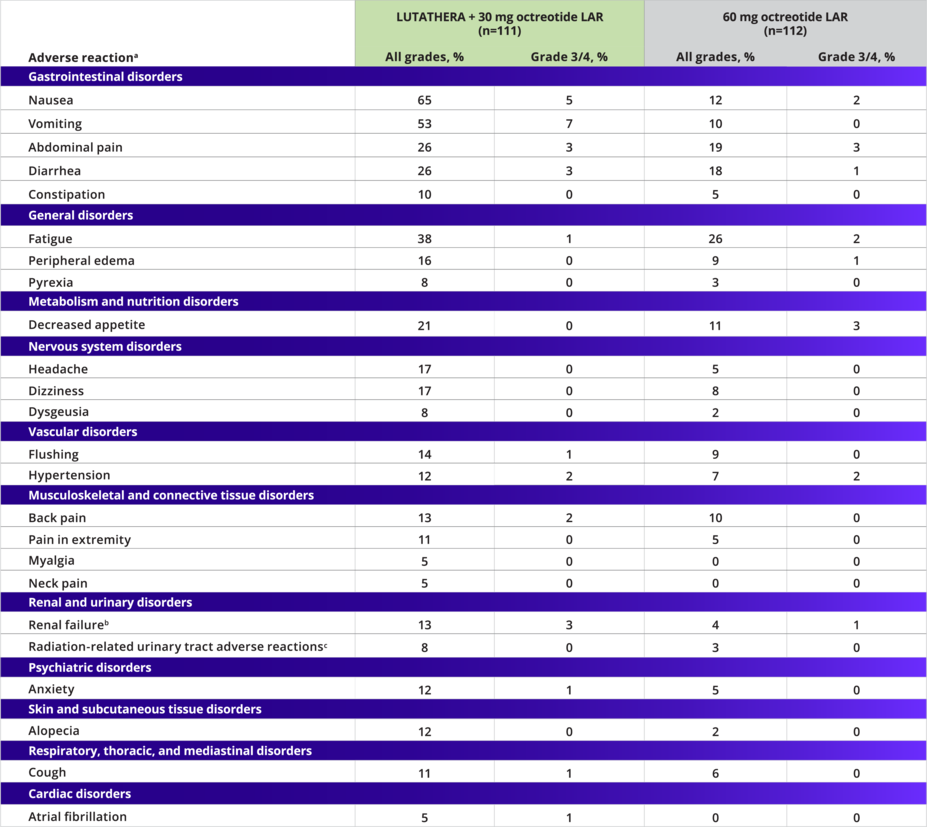
Most adverse reactions seen in the LUTATHERA arm were grade 1/21
Adverse Reactions Occurring at a Higher Incidence in the LUTATHERA Arm (Between-Arm Difference of ≥5% [All Grades] or ≥2% [Grade 3/4])1
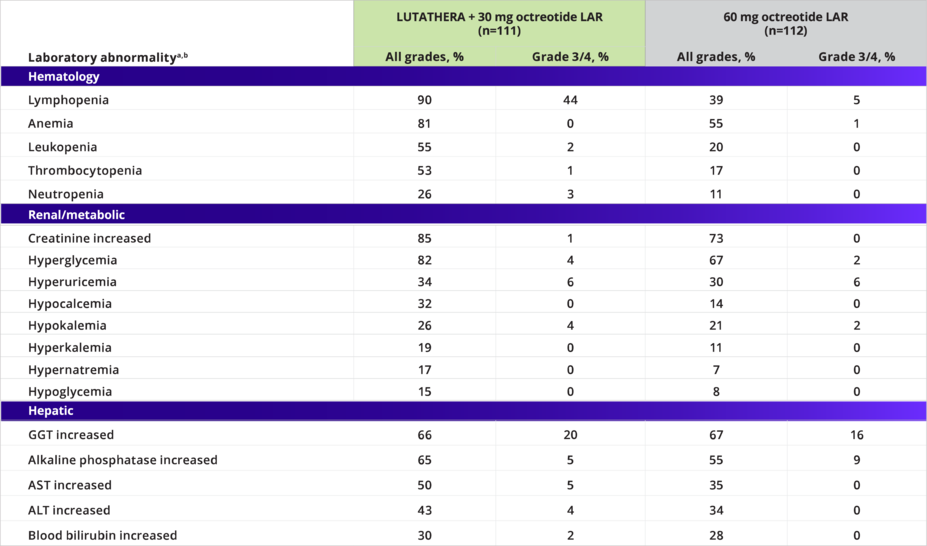
The most common grade 3/4 adverse reactions with a higher incidence in the LUTATHERA arm were lymphopenia (44%), increased GGT (20%), vomiting (7%), nausea (5%), increased AST (5%), increased ALT (4%), hyperglycemia (4%), and hypokalemia (4%)1
aNational Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03. Only displays adverse reactions occurring at a higher incidence in LUTATHERA-treated patients (between-arm difference of ≥5% [all grades] or ≥2% [grade 3/4]).1
bIncludes the terms glomerular filtration rate decreased, acute kidney injury, acute prerenal failure, azotemia, renal disorder, renal failure, and renal impairment.1
cIncludes the terms dysuria, micturtion urgency, nocturia, pollakiuria, renal colic, renal pain, urinary tract pain, and urinary incontinence.1
NETTER-1 Laboratory Abnormalities
LUTATHERA has a well-established safety profile1
Laboratory Abnormalities Occurring at a Higher Incidence in the LUTATHERA Arm (Between-Arm Difference of ≥5% [All Grades] or ≥2% [Grade 3/4])1
7% of patients required a reduced dose and 5% discontinued treatment with LUTATHERA due to AEs2
aValues are worse grade observed after randomization.
bNational Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0.3. Only displays laboratory abnormalities occurring at a higher incidence in patients treated with LUTATHERA (between-arm difference of ≥5% [all grades] or ≥2% [grade 3/4]).
Demonstrated long-term safety at 5 years with no new safety signals reported1,*
Adverse Events | During the long-term follow-up, only serious adverse events (SAEs) deemed related to treatment with LUTATHERA and AEs of special interest (hematotoxicity, cardiovascular events, and nephrotoxicity, regardless of causality) in the LUTATHERA arm were reported3 |
Grade ≥3 Treatment-Related SAEs During the Entire Study | 7 (6%) of 111 patients treated in the LUTATHERA arm3 |
Incidence of Treatment-Related SAEs During the Long-Term Follow-Up Period | 3 (3%) of 111 patients treated with LUTATHERA3 |
MDS or Acute Leukemia | No new cases were reported during long-term follow-up3 |
Diffuse Large B-Cell Lymphoma | One patient developed diffuse large B-cell lymphoma during long-term follow-up that was deemed unrelated to treatment with LUTATHERA3 |
Nephrotoxicity of Grade ≥3, Regardless of Causality | Reported in 6 (5%) of 111 patients in the LUTATHERA arm and 4 (4%) of 112 patients in the control arm during the study3 |
*Cutoff date for final analysis was January 18, 2021.3
aERASMUS study design: Retrospective safety data are available from 1214 patients in ERASMUS, an international, single-institution, single-arm, open-label trial of patients with SSTR+ tumors (neuroendocrine and other primaries). The median duration of follow-up was >4 years.
AEs, adverse events; ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transferase; LAR, long-acting release; MDS, myelodysplastic syndrome; SSA, somatostatin analogue.